Evidence-based Practice in AAC
Dr. Jill Senner and Matthew Baud are staunch advocates for using research-based strategies and other evidence-based practices (EBP) in their AAC work. In today’s post. they share their thoughts on what EBP is, why it is important for AAC professionals, and how to incorporate it into our clinical and educational practices.
their AAC work. In today’s post. they share their thoughts on what EBP is, why it is important for AAC professionals, and how to incorporate it into our clinical and educational practices.
::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::::
Facts Matter: EBP in AAC
Evidence-based practice (EBP) has been a buzz word in healthcare and education for almost two decades. However, “it has been well documented in many disciplines that major gaps exist between what is known as effective practices (i.e., theory and science) and what is actually done (i.e., policy and practice)” (Fixsen et al., 2005, p. 2). What is EBP, why is it important and how can we make sure we’re incorporating evidenced-based practices into our work with students and clients using AAC? Let’s take a look at answers to each of these questions below.
What is EBP?
“Evidence-based medicine is the integration of best research evidence with clinical expertise and patient values.” (Sackett et al., 2000, p.1). Each of the three elements making up the sides of the EBP triangle is equally important. Best research evidence refers to using the most current, well-designed, peer-reviewed research available for clinical decision-making. We can look to research to determine the reliability and validity of assessment instruments we select as well as treatment methods we employ. Clinical expertise (i.e., expert opinion) refers to a practitioner’s cumulative education, experiences, and clinical skills. However, if we only make decisions based on clinical expertise (without considering best evidence or patient values) we’re not using EBP. Reading AAC-related journal articles is a great way to both continue developing clinical expertise and stay informed about best research evidence. Finally, we must consider client and/or caregiver values, interests, needs and choices to be using EBP. 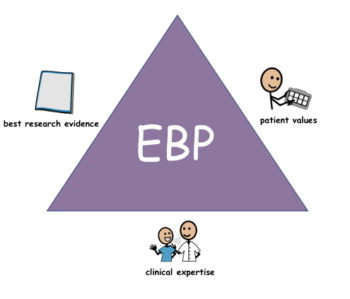
Why is EBP important?
EBP improves quality of care and can protect clients or students from questionable or harmful interventions.
There can be significant negative consequences when the EBP triangle becomes skewed to one side. The following true story provides a cautionary example of clinical expertise overshadowing current best research evidence:
Transorbital lobotomy was a crude procedure used most frequently during the 1940s and 50s. In this procedure, a tool similar to an ice pick was inserted through the eye socket, into the frontal lobe of the brain, and then wiggled around. Despite the lack of evidence supporting the effectiveness of transorbital lobotomy, one man, Walter Freemean, an American neurologist, and psychiatrist, widely promoted this technique as a cure for mental illness. He proposed no candidacy criteria, contraindications, or specific methods. Despite the appearance of articles in the literature suggesting that the procedure could be harmful, Dr. Freeman persisted. By 1951, almost 20,000 men, women, and children had been lobotomized in the United States, many of whom died or suffered permanent brain injury.
As AAC practitioners, we can’t cause death or physical injury by using scientifically questionable techniques, however, our clients can experience negative consequences if an unproven technique prohibits the use of effective and appropriate treatment or displaces other forms of communication.
How to Incorporate EBP into Practice
In the digital age, there are many AAC articles, social media posts, and videos popping up every day. However, not everything we watch or read is based on scientific evidence. It is the position of the American Speech Language Hearing Association (ASHA) that SLPs “incorporate the principles of evidence-based practice in clinical decision making to provide high quality clinical care.” Whether reading something on social media, checking out a video, or attending a presentation, we should always be thinking critically about what we are seeing and hearing. We should be highly skeptical about words such as “always” or “everyone” – AAC is not one-size-fits-all and no one product or treatment is always appropriate for all clients. We can look at the references provided and see if they represent high quality evidence. If no references are provided, we can ask for them or do a quick search of the subject on our own to determine if the research supports or refutes the claims made.
It can be quite time-consuming for busy professionals to regularly read journal articles and keep up with the AAC literature. However, there are time-saving resources that can help clinicians stay abreast of the literature without having to do exhaustive monthly searches:
ASHA has created an online searchable database to help clinicians find articles related to AAC as well as a variety of speech and language disorders that may result in the need for AAC such as autism, apraxia of speech, and ALS. Each entry includes an article summary as well as an evidence rating for the article.
This monthly newsletter summarizes research articles related to practice in speech-language pathology. Many of the articles are relevant to AAC.
The Prentke-Romich Company (PRC) hosts a series of live online meetings to discuss current research in AAC. Two journal articles are reviewed each month by guest presenters and a written summary of each journal article is provided.
References:
https://www.asha.org/research/ebp/
Fixsen, D. L., Naoom, S. F., Blasé, K. A., Friedma, R. M., & Wallace, F. (2005). Implementation Research: A Synthesis of the Literature. Tampa: FL.
Sackett, D. L., Straus, S. E., Richardson, W. S., Rosenberg, W., Haynes, R. B. (2001). Evidence-Based Medicine: How to Practice and Teach EBM, 2nd Ed, Churchill Livingstone, Edinburgh.
About the Guest Authors
Jill E Senner, Ph.D., CCC-SLP is a speech-language pathologist with 20 years of experience working with children with complex communication needs. She is the owner/director of Technology and Language Center where she specializes in providing augmentative and alternative communication (AAC) and assistive technology (AT) services including assessment, consultation and training, and workshops/lectures. Dr. Senner has presented at numerous national assistive technology conferences and has taught graduate courses in AAC and swallowing disorders. She has published research in the areas of AAC, siblings, and disability, and swallowing disorders in cerebral palsy.
Matthew R Baud, MS, CCC-SLP, has been working with AAC for the past 14 years. He currently is the Assistive Technology Coordinator at Niles Township District for Special Education (NTDSE) performing evaluations, training and coaching communication partners. Matthew also has his own AAC private practice working with individuals with complex communication needs from birth through adulthood. He is an adjunct professor at Saint Xavier University where he teaches a graduate course in AAC and has presented at national and state conferences. Matthew has published research in the areas of AAC.
Filed under: Featured Posts, PrAACtical Thinking
This post was written by Carole Zangari