AAC Assessment Corner with Vicki Clarke: The Eyes Have It-Assessment Considerations for High Tech Eye Gaze Access
AA C assessment is an area that most professionals struggle with for one reason or another. I am so grateful to Vicki Clarke for returning to share her thoughts on the prAACticalities of conducting these evaluations. If you are looking for tips on assessing someone who needs high tech eye gaze AAC, this post is for you.
C assessment is an area that most professionals struggle with for one reason or another. I am so grateful to Vicki Clarke for returning to share her thoughts on the prAACticalities of conducting these evaluations. If you are looking for tips on assessing someone who needs high tech eye gaze AAC, this post is for you.
For other posts authored by Vicki, click here.
:::::::::::::::::::::::::::::::::::::::::::::::::::::::::::
The Eyes Have It: Assessment Considerations for High Tech Eye Gaze Access
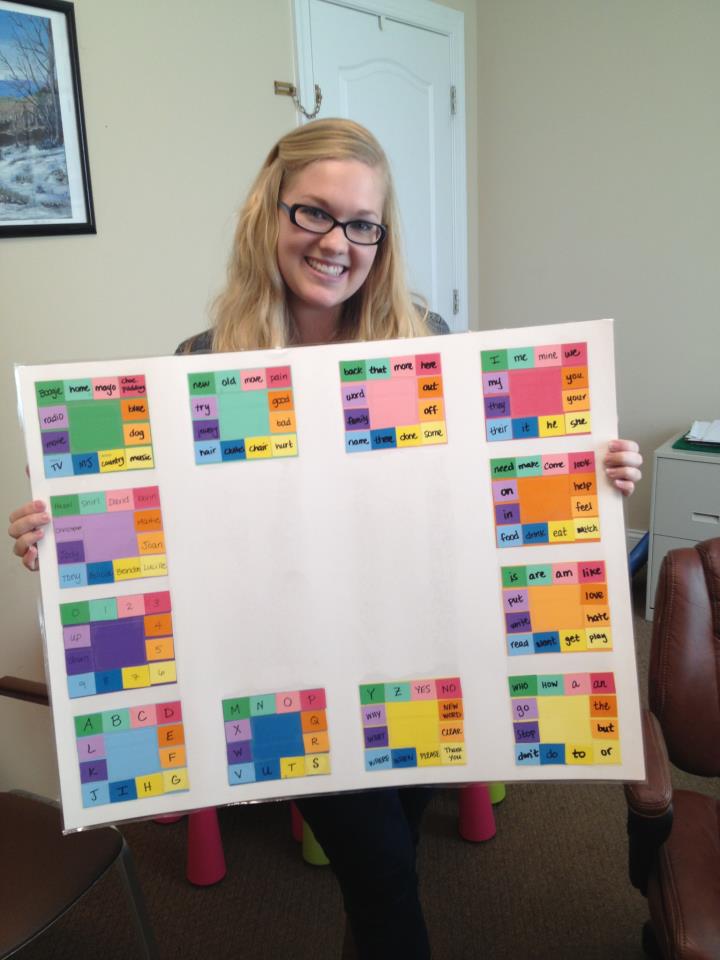
Eye gaze control for AAC device access is a hallmark technological achievement in the world of speech generating devices. For people with significant motor challenges we are no longer limited to scanning as our one choice for AAC access. AAC Specialists have been using light tech eye gaze boards and PVC pipe frames with these friends for years, but now we are able to offer voice output.
Eye gaze is for a much larger audience that we first imagined. Katya Hill (2009) suggested the following clinical populations for eye gaze access application: ALS, Traumatic Brain Injury, Cerebral Palsy, Multiple Scleroses, Muscular Dystrophy, Spinal Cord Injuries and Strokes. In addition, we try eye gaze for any of our students or patients who do not have consistent, comfortable access by touching a screen with their body, those with Cerebral Palsy, Rett Syndrome, and other syndromes causing atypical movement patterns. If a student has to use a stylus or pointer for direct access, we may still give eye gaze a trial, simply to open the door for discussion about all of our options for communication.
Although eye gaze access to speech generating devices is exciting, there are some situations when it is simply not the best choice. There are some challenges with using eye gaze on a high tech device that families need to consider during the evaluation process. There are issues that may negatively impact the ability to use eye gaze access such as movement disorders, certain medications including anticonvulsants or antidepressants and Baclofen; insufficient visual acuity, cataracts, and eye movement problems such as strabismus and nystagmus. Students with cortical visual impairment may have difficulty with visual recognition of symbols and may need highly individualized modifications of the appearance of boards/symbols.
Other difficulties involve the need for a consistent placement of the device in relationship to the patient. Patients have to have mounting systems that allow the device to be positioned correctly in their different seating/lying/standing positions. Students who are ambulatory need to walk to the device and position themselves the correct distance to allow the camera to pick up their eyes. Having an eye gaze device can mean more hours in a particular position than is advised for a patient. Eye gaze devices are heavy, even the new ones. They can be cumbersome to use across environments simply due to the need for partners to set them up for the AAC user.
Although I strongly encourage families to consider eye gaze when it is appropriate, I find it helpful to discuss all of these issues in advance so that families are not disappointed when the miracle AAC device doesn’t solve all communication difficulties. We talk about the need for multimodal communication options, in particular when an eye gaze device is our primary communication method. We talk about the validity in continuing to use our light tech communication methods such as gestures, facial expression, live voice scanning and simple eye gaze frames. At times eye gaze isn’t effective at first, in particular with our students with cortical visual impairment. They need time to develop their visual skills, become familiar with visual symbols and learn eye gaze cause/effect before they can see the symbols sufficiently to make the device work. As we are working on these visual skills, we have to teach language and give access to communication in other ways such as live voice scanning, gestures, switch scanning and, light tech eye gaze boards with recognizable symbols/photos. An eye gaze device might be our end goal but we have to help families understand the, sometimes lengthy, path we may need to travel in our effort to get to the device.
What is required for eye gaze access:
- Sufficient movement control
- Sufficient visual acuity with at least one eye
- Mounting equipment which allows for the device/camera to be positioned precisely for the patient (all axis movement on a mount is best, i.e. the device can be positioned higher/lower/left/right/tilted etc. to capture the reflection from the patient’s eyes best).
- Visual processing skills sufficient for the patient to visually attend to targets on the screen. In practice we’ve found we need a minimum of a .3 second pause on an image to begin to work on eye gaze. That’s a very brief glance, so it’s easy to achieve during initial trials.
What is calibration and why does it matter?
Calibration is the process in which the patient gazes at a moving target on-screen while the cameras and sensors determine the exact properties of the patient’s gaze reflection and position for different areas of the screen. That’s my unscientific explanation, but hopefully you understand that calibration is different for different people so it’s best to get the actual user to calibrate the device. I have heard of people using their own calibration or one of a family member when it was difficult to achieve with a patient. This technique makes sense if it allows us to initially get started, but an individualized calibration is best as soon as possible.
Tricks for calibration:
- For very young students or those with cognitive delays, choose highly motivating targets for calibration. When the device allows you to change the calibration target, choose their favorite video or character to help them attend. One of my favorite calibration targets was a video of little Emma’s daddy telling her to “look this way, Honey!”
- For patients with cortical visual impairment, use their personal visual strategies to make the calibration screen and target most visually accessible. For example, many of our students with CVI achieve visual attention best with a black screen and high contrast image or familiar video.
- Once you have a useable calibration, do NOT drive your student crazy recalibrating. This is a one-time operation that only needs to be done again if you are trying to improve the original calibration. It doesn’t go away when the device is turned off.
- Save an extra copy of the calibration user file so that when someone accidentally recalibrates (they will!) you won’t lose that perfect calibration it took you so long to get.
- A “good” calibration verses a successful “bad” calibration only means that the student will be able to access a smaller point on the screen than if they had a less successful calibration. Students who achieve a less precise calibration will need to have targets that are larger to allow them to be successful, but they can still use the device.
- If the calibration is moving too quickly for your AAC user to establish visual gaze, you can slow the calibration down or use a “keyboard step-through” setting which allows you to choose when to start the calibration on a given area and to move the calibration target to the next location.
- If the AAC user is experiencing difficulty visually attending to certain areas of the screen, you can set a smaller area of screen to use for calibration, for example, you can choose to only use the bottom half of the screen for calibration purposes. The calibration will allow access to the entire screen, even if the calibration is only done on the bottom half of the screen.
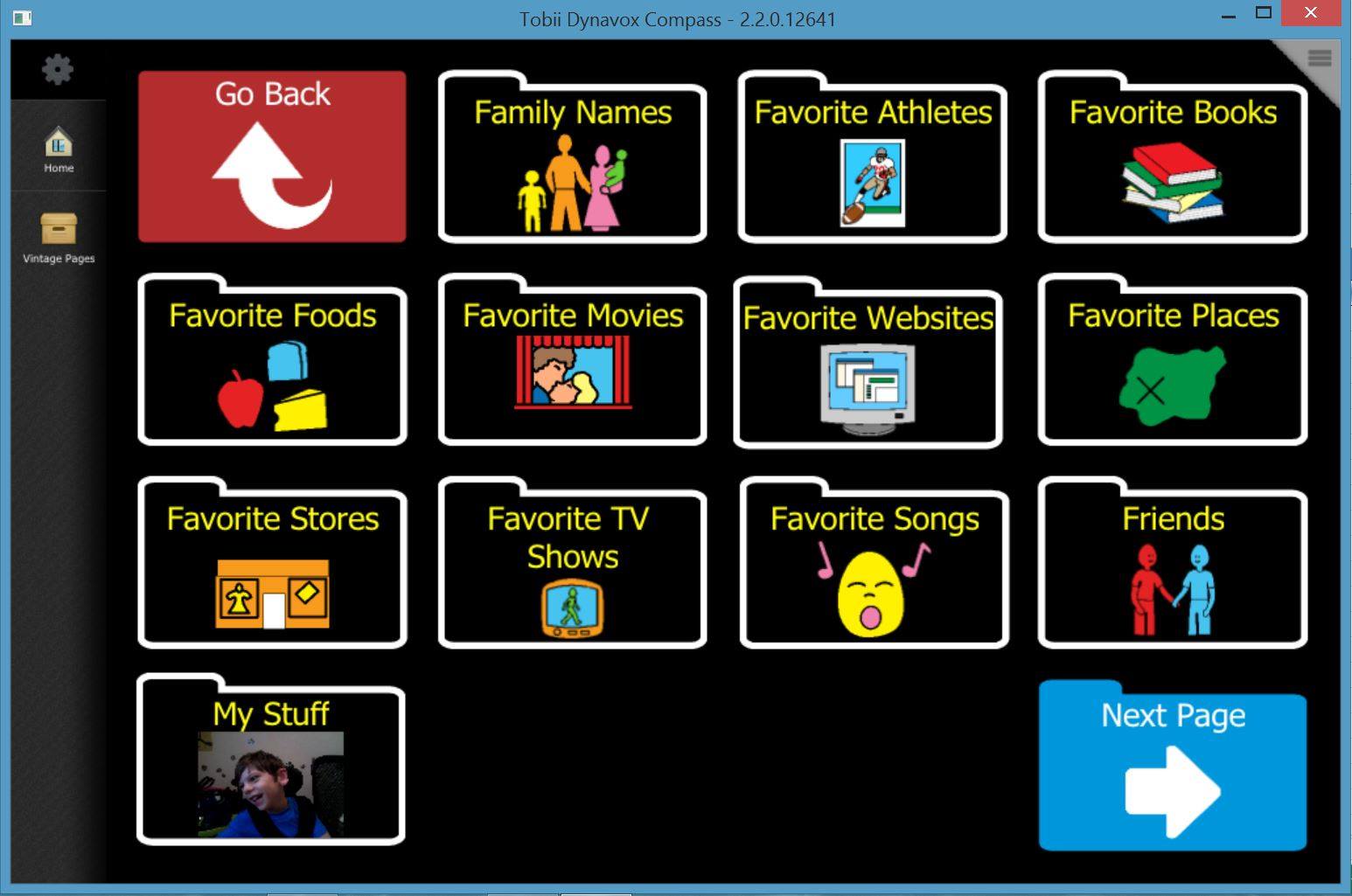
Is there a difference in the how different manufacturer’s eye gaze devices work with different patients? Yes, in my experience, the access differences are primarily in the number of cameras and sensors that are used and how robust the system is. Some devices use 2 cameras and 1 sensor and some use 2 sensors and one camera. In clinical practice I can’t say that we have consistently seen one work better than the other for all patients. We have definitely seen an improvement in reliable eye gaze recognition as the devices’ computer systems have been outfitted with more memory, hard drive capacity and other bells and whistles that new systems have. In general, I would say that if one device is not working well, I’d seek out another one, just to see if there is a difference. If you have tried a system in the past, you might want to revisit eye gaze since the newer, more robust systems have been introduced.
Common Problems:
- Environment- be aware of the effect of lights (natural and artificial) reflecting on the eye and potentially interfering with cameras reading the infrared reflection. Also consider visual distraction for patients with cortical visual impairment. Clinically, I have had the most success using lamp lighting behind the patient with curtains blocking windows for initial evaluation. For patients with cortical visual impairment, I have taken darkening the room to a science with very limited lighting except the device. I only have evidence from my own clinic to support this, but we’ve had nice success with this technique.
- Positioning- make sure that the device is the prescribed distance from the patient. It’s about 21” but is variable device to device, so check. Being too close or too far will impact the student’s success.
- Inappropriate size of targets for the level of calibration achieved- remember that the less accurate the calibration, the larger the targets have to be.
When you are just starting to dabble in evaluation for high tech eye gaze access, invite the sales representatives to join you. We had our sales reps with us for years as we became more comfortable with the details of the different devices.
What tricks and tips do you have to share with us? Leave a comment below so we can compare notes!
Please note, we see AAC users in both school settings and medical settings so I use the terms “patient” and “student” interchangeably when describing our friends.
Resources Consulted:
Hill, Katya, 2009. Evidence Based Principles for Selecting Eye Gaze AAC Technology, Presented at American Speech and Hearing Association Conference, Handout accessed online 4/17/2016 at http://www.asha.org/Events/convention/handouts/2009/1539_Hill_Katya.
Moore, Rachel, Jackie Ayre, Will Wade and Mike Donegan. Presented at ISAAC Conference. Handout accessed 4/17/2016 at http://acecentre.org.uk/Websites/aceoldham/images/Presentations/Experiences%20of%20Eye%20Gaze_8_999.pdf
Special Education Technology- British Columbia (SET-BC)). Eye Gaze System Considerations, accessed online 4/17/2016 at https://www.setbc.org/download/public/Eye_Gaze_System_Considerations.pdf
Filed under: Featured Posts, PrAACtical Thinking
Tagged With: assessment, eye gaze
This post was written by Carole Zangari

11 Comments
Thank you for this great post! I’m about to begin a communication journey with a young child who is just entering preschool and has CP and CVI diagnoses. I will be sharing this article with her team as we discuss communication options and get started with the process of finding the right support and tools for her needs.
Such an exciting time! I have a little bitty with the same diagnosis at the same stage right now. Challenging and fun to be on this journey.
It can be so difficult to explain why the “magic” of high-tech eye-gaze, doesn’t always translate to a perfect communication solution. This lays out the myriad of considerations for eye-gaze so nicely! Thank you!
I’m so glad it is helpful. Families are just so hopeful about eye gaze that it’s hard to keep them encouraged when they don’t see success. I think if we can explain the details clearly, have acceptable alternatives and a long term plan we can keep everyone positive and moving forward!
Very helpful article for myself as a therapist new to eye gaze – thanks!
You’re welcome! Enjoy your new journey. This is an exciting and dynamic field that has never failed to challenge me, even after several decades of practice!
I have a student who has the motor capabilities to make direct selections with their hands in a field of 2-4 with icons/picture cards as small as 3×3″, but does not do so consistently and only when extremely motivated. I’ve been trialing an eye gaze device with her and she has made enormous gains. She has expanded her vocabulary and has shown the ability to communicate medical info as well. What are your thoughts on available access methods versus success and consistency? I want to move forward with the eye gaze device but I feel odd about it since she is able to move her arms. However she has been far more successful with this device and access method. Any thoughts would be appreciated!
Hi Becca,
In making a choice between different access methods, I try to go with the least effortful, most natural and most successful option. I find that patients often want to touch the device if they can, but if she is having so much more success with eye gaze, she may be very happy to have the eye gaze access. One nice thing abut these devices, is that they have multiple access options. You can go with the eye gaze system but still use it with touch access if she wants to use a different method one day (or if she wants to switch up during the day- fatigue?). The biggest negative is the consistent positioning needed and the weight of the device. They are getting lighter though and more tolerant of movement and position. Best of luck with your choice! Your student is lucky to have a therapist who is being so thoughtful for her!
What do you consider to be minimum requirements for eye gaze technology? Being able to track? Look at an object/picture for 3 seconds? Asking for a SCI student with TBI.
HI Vicki
I just started treating an individual on eyegaze technology for approx. 3 years but noticed several factors that are affecting his access (fatigue and stamina). Patient clearly knows what he is asked to do but is inconsistent. As a result, he often is discouraged and gives up. I encouraged multimodal communication but getting resistance from the team as they are fearful patient will regress with using eye gaze technology. Do you know of parent friendly resources, articles or antidotal notes I can share with the team about using all modalities…(specifically to individuals who use eye gaze technology)?
At the request of administrators, I am looking for some academic tests that can be accessed via eye gaze technology. I have access to a variety of software from Inclusive TLC, SmartBox etc. I have created some of my own through the use of ChooseITMaker. Administrators are looking for more common and standardized assessments. Any Suggestions?